MPFL Case Discussion
MPFL
Reconstruction Case Presentation
Introduction & Background:
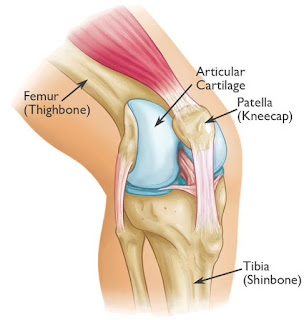
The
medial patellofemoral ligament (MPFL) is a band of retinacular tissue connecting the femoral medial epicondyle to the
medial edge of the patella. The MPFL is approximately 55 mm long, and its width
has been reported to range from 3 to 30 mm. The MPFL is overlaid by the distal
part of vastus medialis obliquus to a variable extent, and fibers of MPFL merge into the deep aspect of the muscle. Despite
the MPFL being very thin, it had a mean tensile strength of 208 N, and has been reported to be the primary
passive restraint to patellar lateral displacement. Lateral patellar
displacement tests in vitro showed that the patella subluxed most easily at 20 degrees knee flexion. The contribution
of the MPFL to resisting patellar lateral subluxation was greatest in the
extended knee.
Anatomy:
Classification:
·
Wiberg type 1 or a
o
roughly
symmetrical facets
o
concave
facets
o
equally
sized facets
o
although
presumably the ideal shape of the patella, it is in fact rather uncommon, occurring
in only 10% of the general population
·
Wiberg type 2 or b
o
slightly smaller size of the medial facet
o
concave
aspect of the lateral facet
·
Wiberg type 3 or c
o
markedly smaller size of the medial facet
o
more
vertical orientation of the medial facet
Patella
was classified according to Baumgartl’s classification:
·
Type I patella: medial and lateral facets,
both are concave with equal length
·
Type II patella: lateral facet is more
prominent compared to the medial facet; medial facet is plane or concave.
·
Type III patella: a smaller and convex medial
facet.
·
Type IV patella: no medial facet or central
rim; as also called “Jokey hat”.
The
Outerbridge MRI grading system was used for the degree of patellar
chondromalacia
·
Grade 0: Normal.
·
Grade I: “Softening” or edema in the
cartilage without contour irregularity.
·
Grade II: Surface irregularity, fissure or
focal defect in less than 50%
·
Grade III: Fragmentation, fissure, or defect
formation in 50% or more of the cartilage
·
Grade IV: Full thickness loss up to the bone
and reactive changes in the subchondral bone
Classification
of trochlear dysplasia (Dejour et al)
·
Type A: normal
shape of the trochlea, but a shallow trochlear groove
·
Type B: markedly flattened or even
convex trochlea
·
Type C: trochlear facet asymmetry, with
too high lateral facet, and hypoplastic medial facet
·
Type D: type C features and a vertical
link between facets ('cliff pattern')
Patient Information:
Ø Patient
- ‘X’
Ø Age
- 22 years/ Male
Ø Date
of Admission: 10/04/2019
Ø Date
of Surgery: 11/04/2019
Chief
Complaint:
The patient had pain over the left knee (knee
cap). The patient had recurrent lateral patellar dislocation of the left knee.
History of Illness:
The patient
had a recurrent
patellar dislocation and the patient
feels instability of knee cap (patella) while flexing
the left knee since fall. The patient
gave a history of slip and fall at work
in 2015 and December 2018.
After the injuries, the patient took
treatment in the nearby polyclinic. The patient had
undergone conservative treatment but the conservative treatment didn’t help the
patient. The patient contacted our hospital for further management(surgical
treatment). The patient was
examined by traumatologist and got admitted in the traumatology department. X-ray was taken
and it showed no fracture of the patella.
v Previous
Injury: The patient gave a history
of the patellar dislocation
in 2015- 2 times.
in 2018- 4 times.
v Developmental
History: No any developmental histories
v Drug
History: No known drug allergies. The patient is not on
treatment for CVS.
v Past
Medical History: The patient gave a past medical history of Synovitis of the left knee with the chronic instability of the knee
No Diabetes mellitus; No Asthma; No
thyroid disease.
v Past
Surgical History: Joint aspiration of left knee & No
any blood transfusion.
On Examination:
Patient is conscious, oriented.
Vital Signs:
· BP
– 120/80 mmHg
· PR
– 80/min
· SPO2
– 99%
Local Examination:
· Pain
and chronic instability over the left patellar region are present.
· Grasshopper
sign +ve
· Positive “J” sign
· Patella
glide test >2
· Patellr
grind test +ve
· Insall-Salvati
2.1
· Tibial
Tuberosity – Tibial Groove (TT-TG) – 11.20mm
· Positive
apprehension test.
· Active
toe movements present.
· Distal
pulse present.
MRI
Findings:
TT-TG – 11.20mm
Preparation:
Patient in Supine position: Place the patient on a radiolucent table. An adjustable Knee and Tibial
Positioner kept beneath the lower extremity.
Procedure:
1.
Arthroscopic debridement of the left
knee.
2.
AMTT (AnteroMedial Tibial Tuberosity) with distalization of the left knee.
3.
MPFL reconstruction of the left
knee.
1. The patient under spinal anesthesia, place a tourniquet on the upper thigh.
After sterile preparation and drapping, arthroscopy of the left knee joint was
performed through standard anteromedial and anterolateral portals. During the
procedure lateral positioning of the patella 2nd stage,
chondromalacia patella was revealed. Medial and lateral meniscus, ACL and PCL
were not found damaged. Thorough wound washes given. Arthroscope removed.
Aseptic bandage gave.
2. The patient under spinal anesthesia, after processing
the operative field, access to the area
of the proximal tibial tuberosity was performed with the longitudinal incision. The incision is made
from the superior tip of the patella to
the tuberosity of the supracondylar of the
femur up to 5cm.
After the subcutaneous lateral retinacular release of the patella, an osteotomy
of the tibial tuberosity was performed. Then the anterior tibial tuberosity was
moved medially with distalization, was fixed with 2 cortical screws.
3. From the same incision of the skin and underlying tissues in the
projection of the “Pes Anserinus”, the ST tendon was found and separated, and
the ST-G autotransplant was taken up to 20cm in length using a stripper.
Over the upper 3rd of
the medial edge of the patella 2cm length of the channel has been madewith 4.5
mm drill, through which the graft of MPFL was transplanted.
After an additional incision of up to 2cm in length in the area of
attachment of MPFL in the medial condyle of the femur,
7mm channel is formed, through which the autograft has been drawn and
tightened, the autograft is then fixed with 9mm BIOSURE SCREW.
Thorough wound washes given. Wound closed in layers. Estimated blood loss
150ml. Compression bandage has been given. Immobilization did with a knee
brace.
CLASSIFICATION:
The above
patient condition classified:
Ø According to Wiberg
- Type 2 or b
Ø According to Baumgartl’s classification - Type II patella
Ø According to Outerbridge MRI grading system was
used for the degree of patellar chondromalacia – Grade II
Ø According to Dejour et al – Type C
CONCLUSION:
Ø Surgical
reconstruction, good anatomical reduction, and
internal fixation help to recover the
full range of movements.
Ø Stability
is restored.













Comments
Post a Comment
Thank you for your kind words and your support.